Can You Take ADHD Medication During Pregnancy? Understanding the Risks, Benefits, and Making the Best Choice for You

This page focuses on one question:
Is it safe to take ADHD medication during pregnancy, and how do women make this decision responsibly?
This page does not tell you what to do.
It explains what is known, what is often misunderstood, and how to approach the decision without fear, shame, or pressure.
Why This Question Is So Stressful for ADHD Women
Many ADHD women face this question while planning a pregnancy or after finding out they are already pregnant.
For some, pregnancy is planned.
For others, it is not. Nearly half of all pregnancies are unplanned, and research suggests this number is higher among women with ADHD.
Medication decisions are often framed as simple or moral choices.
In reality, they are medical decisions that require individualized risk–benefit analysis.
Asking this question is not a sign of irresponsibility.
It is a sign that you are taking both your health and your baby’s health seriously.
What the Research Actually Says
Research on ADHD medication during pregnancy has expanded significantly over the last decade.
Stimulant Medications
Examples include methylphenidate and amphetamine-based medications.
Large population studies generally show:
-
no increased risk of major congenital malformations overall
-
no consistent increase in perinatal death or major obstetric complications
Some newer studies suggest:
-
a small possible increase in specific cardiac differences (such as ventricular septal defects) associated with methylphenidate
-
the absolute risk remains low
-
monitoring, such as fetal echocardiography, may be recommended in some cases
Non-Stimulant Medications
Examples include atomoxetine.
-
Data is more limited
-
Available studies do not show large increases in major congenital malformations
-
Smaller sample sizes mean uncertainty remains
This is why decisions are individualized rather than universal.
What Is Often Left Out of the Conversation
A critical piece is frequently missed:
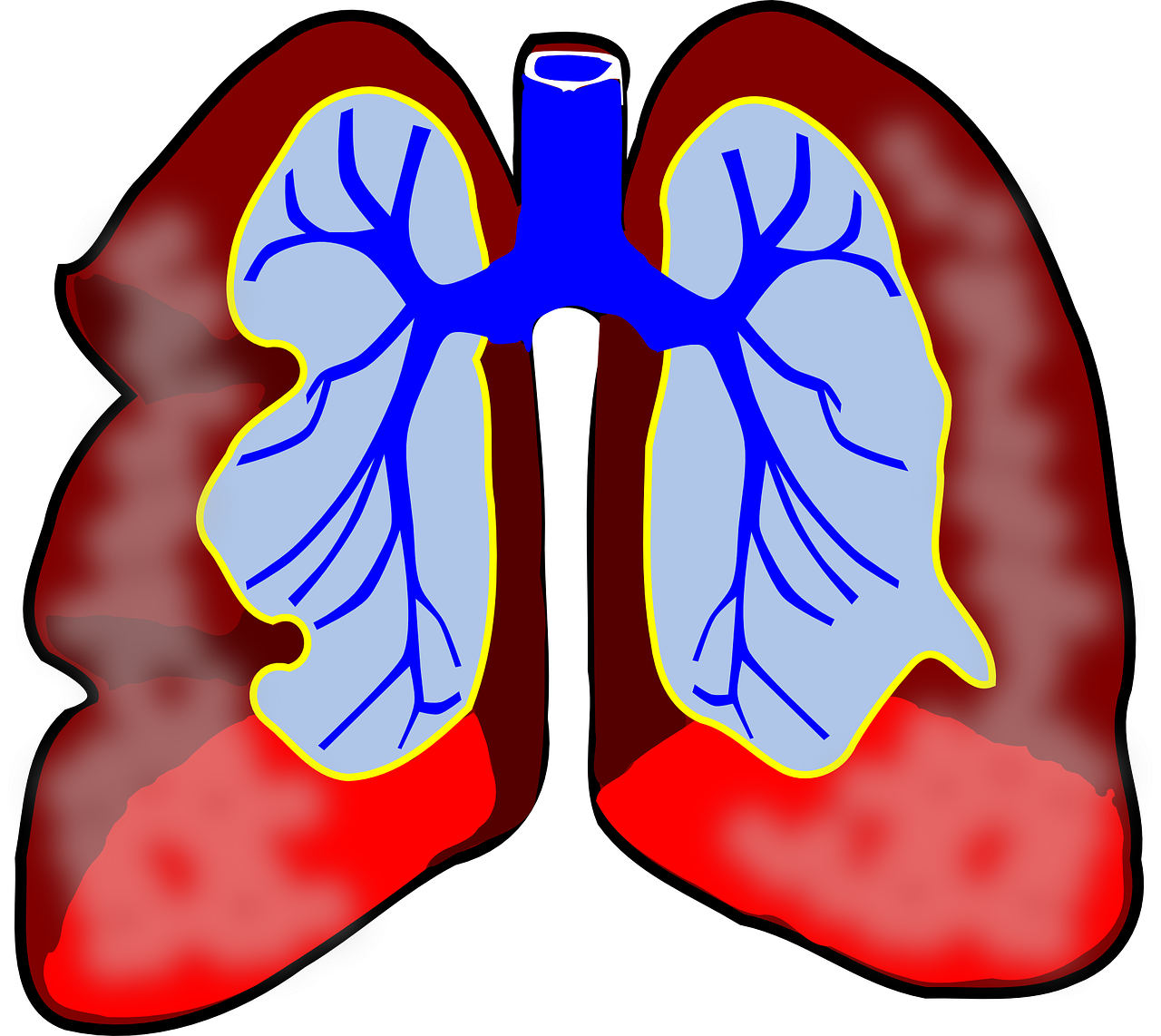
Untreated ADHD can also carry risk.
Severe ADHD symptoms during pregnancy may affect:
🔵 driving safety
🔵 stress hormone levels
🔵 sleep quality
🔵 nutrition
🔵 emotional regulation
🔵 follow-through with prenatal care
For some women, stopping medication leads to:
-
increased anxiety or depression
-
emotional dysregulation
-
impaired daily functioning
-
reduced safety and stability
Medication decisions are not about choosing “risk” versus “no risk.”
They are about choosing which risks are better managed.
Why Some Women Choose to Continue Medication
Some ADHD women decide to continue medication because it:
🔵 supports daily functioning and safety
🔵 reduces emotional overwhelm and stress
🔵 helps maintain routines, appointments, and prenatal care
🔵 protects mental health stability
For these women, medication is part of maintaining a regulated nervous system during a demanding physiological transition.
Why Some Women Choose to Pause Medication
Other women choose to stop medication because:
🔵 they feel comfortable managing symptoms with supports
🔵 their ADHD symptoms feel milder during pregnancy
🔵 they prefer non-pharmacological approaches
🔵 they want to minimize medication exposure
This choice can also be appropriate.
There is no universally correct decision.
How to Make the Decision Safely and Responsibly
Effective decision-making is collaborative and ongoing.
Helpful steps include:
🔵 discussing symptom severity and history with your provider
🔵 reviewing up-to-date research together
🔵 considering mental health risk if medication is stopped
🔵 planning monitoring if medication is continued
🔵 seeking a second opinion when needed
Providers with experience in perinatal psychiatry or ADHD in women can be especially helpful.
Breastfeeding and ADHD Medication
Many ADHD women are told to stop medication entirely while breastfeeding.
Evidence does not support a blanket rule.
Some ADHD medications may be compatible with breastfeeding at low doses, depending on:
-
the medication
-
timing
-
infant health
-
maternal mental health needs
Stability, sleep, and emotional regulation matter for infant safety too.
This decision should be individualized and revisited as circumstances change.
A Neurodivergent-Affirming Reframe
Taking ADHD medication during pregnancy is not about convenience.
Stopping medication is not about virtue.
This is about supporting a nervous system that already works harder, during a period of intense hormonal, physical, and cognitive change.
Informed care respects both maternal mental health and fetal development.
Where This Page Fits
This page focuses only on medication decisions.
You may also want to read:
Resources:
Could this information help someone you know? Share it with your community!
References
Baker, A. S., & Freeman, M. P. (2018). Management of attention deficit hyperactivity disorder during pregnancy. Obstetrics and Gynecology Clinics of North America, 45(3), 495–509. https://doi.org/10.1016/j.ogc.2018.04.010
Bröms, G., Hernandez-Diaz, S., Huybrechts, K. F., Bateman, B. T., Reardon, P., Broe, A., Furu, K., Gíslason, T., Heiskanen, T., Källén, B., Kieler, H., Murray, E., Nielsen, H. S., Pasternak, B., Reichenberg, A., Svanström, J., & Wogelius, P. (2023). Atomoxetine in early pregnancy and the prevalence of major congenital malformations: A multinational study. The Journal of Clinical Psychiatry, 84(1), 22m14430. https://doi.org/10.4088/JCP.22m14430
Kittel-Schneider, S., Quednow, B. B., Leutritz, A. L., McNeill, R. V., & Reif, A. (2021). Parental ADHD in pregnancy and the postpartum period - A systematic review. Neuroscience and Biobehavioral Reviews, 124, 63–77. https://doi.org/10.1016/j.neubiorev.2021.01.002
Scoten, O., Tabi, K., Paquette, V., Carrion, P., Ryan, D., Radonjic, N. V., Whitham, E. A., & Hippman, C. (2024). Attention-deficit/hyperactivity disorder in the perinatal period. American Journal of Obstetrics & Gynecology, 24A. Retrieved July 2024, from https://www.ajog.org
Medical Disclaimer
This content is provided for educational and informational purposes only and is not a substitute for individualized medical advice, diagnosis, or treatment.
ADHD, pregnancy, and medication decisions are complex and vary based on personal medical history, symptom severity, and individual risk factors. Always consult with a qualified healthcare provider, such as an obstetrician, psychiatrist, or primary care clinician, before making changes to medication, treatment, or care plans.
Nothing on this page is intended to replace a collaborative, individualized discussion with your healthcare team.