✨ Title: “The Hidden Link Between Stress, Hives, and Neurodivergence: How Stress Affects the Skin in Neurodivergent Individuals”
Does Your Skin Flare Up When You're Stressed?
You’re not alone. Stress can trigger physical reactions like hives, eczema, or itchy skin. For neurodivergent individuals, the connection between stress and skin health can be even stronger.
Take Jessica, for example. She’s an ADHD client I worked with who experienced mysterious hive outbreaks. After tracking her symptoms, Jessica realized that emotional stress and sensory overload—like loud noises and bright lights—were contributing to her flare-ups.
Jessica's skin began clearing up by taking sensory breaks, improving sleep, and reducing daily stressors.
Her experience isn’t rare. Research shows that ADHD and autistic individuals are more likely to experience stress-induced skin conditions, such as hives and eczema. This unique link between neurodivergence and skin reactions requires a more holistic skincare and stress management approach.
🧠 The Brain-Skin Connection
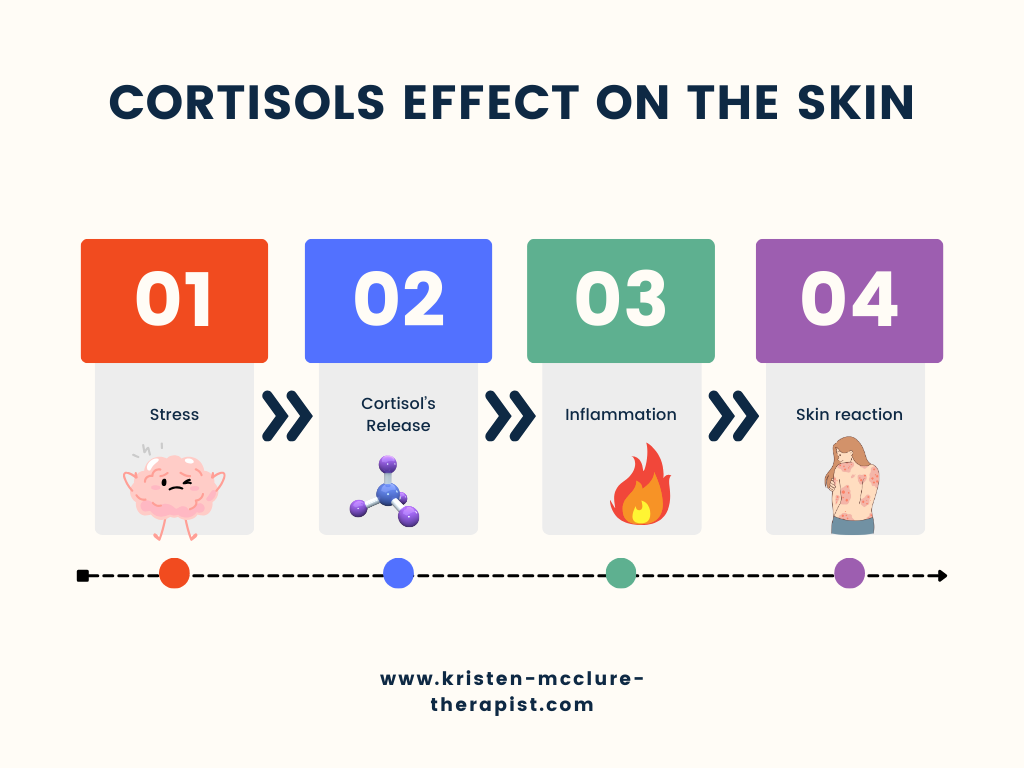
Your skin and brain are closely connected. When stressed, your body releases chemicals like cortisol and substance P.
- Cortisol increases inflammation, worsening skin conditions.
- Substance P (a neuropeptide released during stress) directly stimulates skin cells, leading to itching, redness, and swelling.
Research shows that substance P is released at higher levels in neurodivergent individuals, likely due to heightened sensory processing and emotional dysregulation. This makes their skin more reactive than neurotypical individuals.
Another factor is the role of IL-31 and IL-33, inflammatory cytokines in skin and immune responses. Studies indicate that atopic dermatitis (AD)—more common in ADHD and autism—is linked to these cytokines. Interestingly, IL-31 and IL-33 also contribute to neuroinflammation, meaning skin flare-ups may worsen overall stress responses.
1. Immune System and Skin Flare-Ups
Stress can over-activate the immune system, leading to histamine release. In neurodivergent individuals, this overreaction can cause conditions like hives, eczema, or chronic rashes. Brain stress can directly influence skin health since the immune and nervous systems are intertwined .
What this means: By managing immune health and reducing stress, you can improve both skin and brain function.
2. Sensory Overload and Skin Reactions
Neurodivergent individuals—especially those with ADHD and autism—often experience heightened sensory sensitivities. Stress from sensory overload (like bright lights, loud sounds, or uncomfortable textures) can trigger skin flare-ups.
In addition, emotional dysregulation caused by these triggers adds to the body’s stress load, exacerbating skin conditions.
What this means: Combining sensory-friendly strategies (like noise-canceling headphones or soft clothing) with stress management can help reduce skin reactions.
3. Anxiety, PTSD, and Skin Health
Anxiety and PTSD can manifest physically in the form of hives, flushing, or eczema. These conditions activate the fight-or-flight response, flooding the body with cortisol and histamine.
Neurodivergent individuals may experience more intense anxiety or PTSD symptoms, further impacting their skin and overall well-being.
What this means: Reducing anxiety through grounding techniques, therapy, or mindfulness can ease skin-related symptoms.
4. Other Neurodivergent Traits and Skin Health
Conditions like OCD and Tourette's can also affect skin health. Repetitive behaviors (like skin-picking or tics) and emotional dysregulation may lead to skin irritation, infections, or scarring.
What this means: Addressing these traits with tailored interventions can reduce their impact on skin health.
🦠 Mast Cell Activation and Skin Flare-Ups
Mast cells are immune cells that release histamine during stress or allergic reactions. In conditions like Mast Cell Activation Syndrome (MCAS), which is common in neurodivergent populations, mast cells become overactive, causing frequent hives, flushing, or skin inflammation.
What this means: If you suspect MCAS, consult with a doctor about antihistamines or other treatments that may help.
🥗 Gut Health and Skin
Your gut, brain, and skin are all interconnected. Neurodivergent individuals frequently deal with gut issues like IBS or food sensitivities, which can lead to increased inflammation and skin problems.
Stress disrupts gut bacteria, worsening inflammation and affecting skin health.
What this means: Eating gut-friendly foods like yogurt, whole grains, and leafy greens may balance your gut microbiome and support healthier skin.
🌿 Tips for Managing Stress and Skin Health
If stress is affecting your skin, here are some simple strategies to try:
1. Track Triggers:
- Keep a journal of when skin reactions occur.
- Write down what you were doing, eating, or feeling to identify patterns.
2. Create Calm Spaces:
- Use sensory aids like weighted blankets, soft lighting, or noise-canceling headphones to reduce sensory overload.
3. Stick to a Routine:
- Regular sleep, exercise, and meals help regulate cortisol levels and reduce stress.
4. Choose Skin-Friendly Products:
- Use hypoallergenic, fragrance-free skincare to minimize irritation.
5. Support Gut Health:
- Add probiotic and anti-inflammatory foods (like yogurt, salmon, and vegetables).
6. Practice Stress Tools:
- Try mindfulness apps, biofeedback, or breathing exercises to manage stress.
🌞 Your Next Steps If you believe stress is contributing to your skin issues, start by:
- Tracking symptoms.
- Reducing sensory overload.
- Prioritizing rest.
If the issue persists, consider speaking with a therapist or dermatologist familiar with neurodivergent care.
👉 You deserve to feel good in your skin—inside and out. Take the first step today!
👉 You deserve to feel good in your skin—inside and out. Take the first step today!
📚 References (APA):
- Chung, M. C., Symons, C., & Gilliam, J. (2010). The relationship between posttraumatic stress disorder, psychiatric comorbidity, and personality traits among patients with chronic idiopathic urticaria. Comprehensive Psychiatry, 51(1), 55-63.
- Grossbart, T., & Sherman, P. S. (2009). Skin deep: A mind-body program for healthy skin. Health Press NA Inc.
- Houck, C. (1996). When stress gets under your skin. Good Housekeeping, 222(5), 52.
- Lydon, S., Healy, O., Reed, P., Mulhern, T., & Hughes, B. M. (2017). Health complaints in children with autism spectrum disorder: A meta-analysis. Journal of Autism and Developmental Disorders, 47(8), 2855-2867.
- Malhotra, S. K., & Mehta, V. (2008). Role of stressful life events in induction or exacerbation of psoriasis and chronic urticaria. Indian Journal of Dermatology, Venereology, and Leprology, 74(6), 594-599.
- Robertson, S. M. (2010). Neurodiversity, quality of life, and autistic adults. Disability Studies Quarterly, 30(1).
- Critchley, H. D., Daly, E. M., Bullmore, E. T., & Brammer, M. J. (2000). Neural activity in the anterior cingulate during the experience of autonomic arousal. NeuroImage, 13(6), 1203-1214.


