ADHD and Your Period: Navigating Hormonal Changes
Table of Contents
Toggle
What This Page Covers
How does the menstrual cycle affect ADHD symptoms, and what actually helps?
I
ADHD and the Menstrual Cycle
Many ADHD women notice that their symptoms change predictably across the month. Focus, energy, emotional regulation, sleep, and medication response may improve at certain times and worsen at others.
These shifts are driven by normal hormonal changes across the menstrual cycle, not by effort, motivation, or coping skills.
Understanding this pattern allows you to plan support instead of reacting in crisis.
(For a broader overview of how hormones interact with ADHD across the lifespan, see ADHD and Hormones.)
How the Menstrual Cycle Affects ADHD
The menstrual cycle includes predictable hormonal phases. Each phase can influence ADHD symptoms differently.
Follicular Phase (Cycle Days ~1–14)
Estrogen gradually rises.
Many ADHD women notice:
-
Improved focus and working memory
-
Increased motivation and energy
-
Better emotional regulation
This phase often supports planning, decision-making, and complex tasks.
Ovulation (Mid-Cycle)
Estrogen peaks.
Some women experience:
-
Strong focus and confidence
-
Increased impulsivity or risk-taking
-
Heightened emotional intensity
This is a common time for overcommitting or underestimating limits.
Luteal Phase (Cycle Days ~15–28)
Estrogen drops and progesterone rises.
This phase is often the most challenging for ADHD women.
Common experiences include:
-
Brain fog
-
Increased forgetfulness
-
Lower frustration tolerance
-
Worsened emotional reactivity
-
Reduced medication effectiveness
This is not a failure phase. It is a low-buffer phase.
Menstruation
Hormone levels are lowest.
Some women feel relief. Others feel depleted or foggy. Energy often begins to reset.
Why ADHD Symptoms Feel Worse Late in the Cycle
ADHD brains rely heavily on dopamine for attention, motivation, and executive function. Estrogen supports dopamine signaling.
When estrogen drops:
-
Cognitive load increases
-
Emotional regulation requires more effort
-
ADHD strategies that worked earlier may fail
This is a physiological shift, not a psychological one.
ADHD, PMS, and PMDD
Many ADHD women experience premenstrual symptom worsening. Some meet criteria for PMDD, a severe hormone-related mood disorder.
If premenstrual symptoms include:
-
Marked depression or anxiety
-
Extreme irritability
-
Suicidal thoughts
-
Rapid relief once menstruation begins
This may indicate PMDD rather than typical PMS.
→ See ADHD and PMDD for diagnosis and treatment guidance.
Practical Ways to Support ADHD Across Your Cycle
1. Track Patterns, Not Perfection
Track:
-
Energy
-
Focus
-
Mood
-
Medication response
You are looking for patterns, not daily accuracy.
2. Plan With Your Cycle
-
Schedule demanding work during higher-estrogen phases
-
Reduce cognitive load during the luteal phase
-
Avoid major decisions late-cycle when possible
Planning is accommodation, not avoidance.
3. Externalize Executive Function
Late-cycle ADHD often requires more structure:
-
Visual reminders
-
Written steps
-
Reduced multitasking
-
Fewer decisions
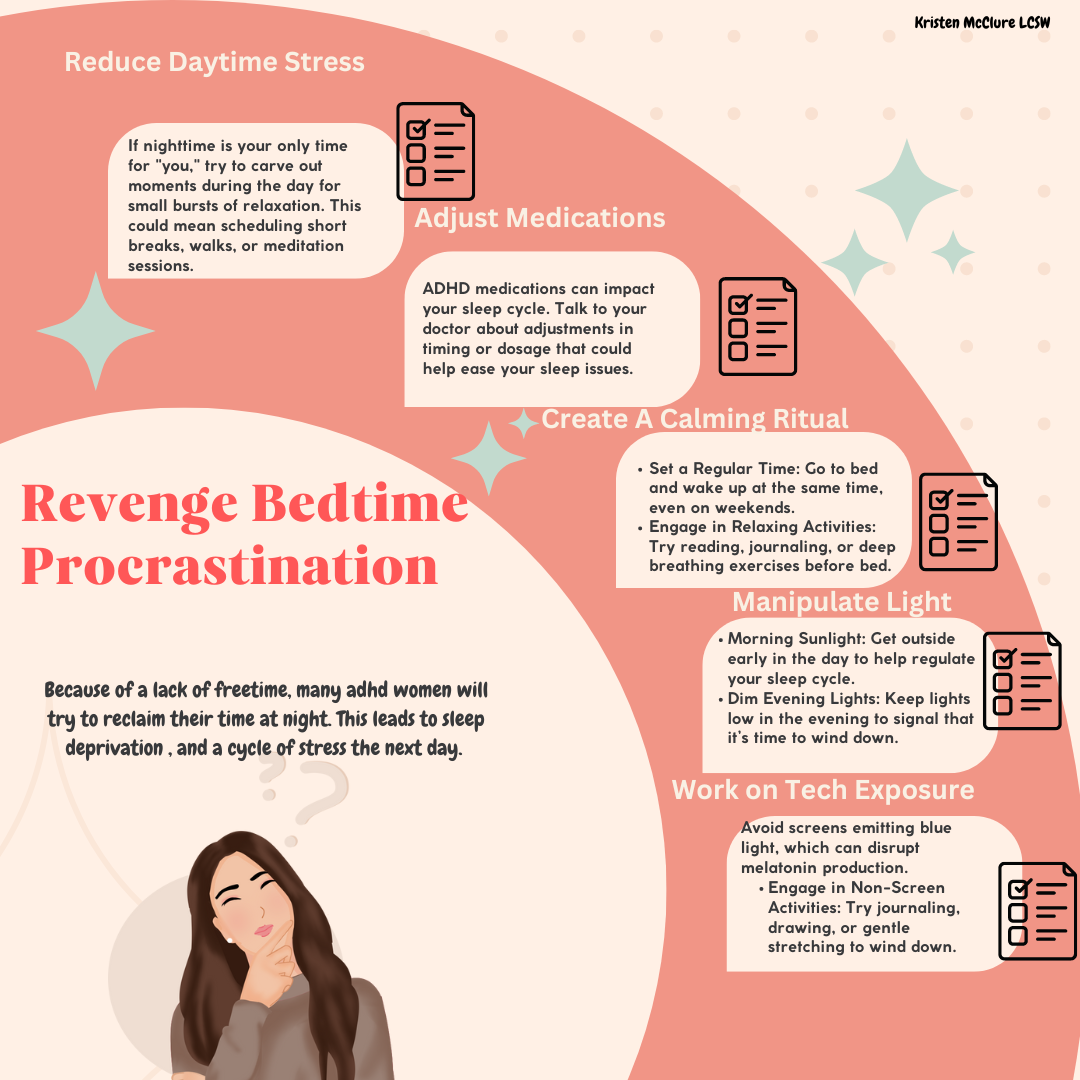
4. Review Medication Timing
Some women notice reduced medication benefit during the luteal phase. Prescribers may consider:
-
Timing adjustments
-
Temporary dose changes
These decisions should always be individualized.
When to Seek Additional Support
Consider further evaluation if you experience:
-
Severe cyclical mood changes
-
Repeated functional impairment late-cycle
-
Depression or anxiety that resolves with menstruation
-
Medication suddenly feeling ineffective every month
These patterns are clinically meaningful.
A Neurodivergent-Affirming Reframe
Your ADHD symptoms are not inconsistent.
Your nervous system is responding to changing conditions.
Learning your cycle allows you to work with your brain, not against it.
Related Resources
References and Research for ADHD and Your Period
- Eng, A. G., Nirjar, U., Elkins, A. R., Sizemore, Y. J., Monticello, K. N., Petersen, M. K., Miller, S. A., Barone, J., Eisenlohr-Moul, T. A., & Martel, M. M. (2024). Attention-deficit/hyperactivity disorder and the menstrual cycle: Theory and evidence. Hormones and Behavior, 158, 105466. https://doi.org/10.1016/j.yhbeh.2023.105466
- Roberts, B., Eisenlohr-Moul, T., & Martel, M. M. (2018). Reproductive steroids and ADHD symptoms across the menstrual cycle. Psychoneuroendocrinology, 88, 105–114. https://doi.org/10.1016/j.psyneuen.2017.11.015
- Bürger, I., Erlandsson, K., & Borneskog, C. (2024). Perceived associations between the menstrual cycle and Attention Deficit Hyperactivity Disorder (ADHD): A qualitative interview study exploring lived experiences. Sexual & Reproductive Healthcare, 40, 100975. https://doi.org/10.1016/j.srhc.2024.100975