
Adhd and Postpartum Depression
Postpartum depression affects many new mothers.
In ADHD women, it is substantially more common and often more disabling.
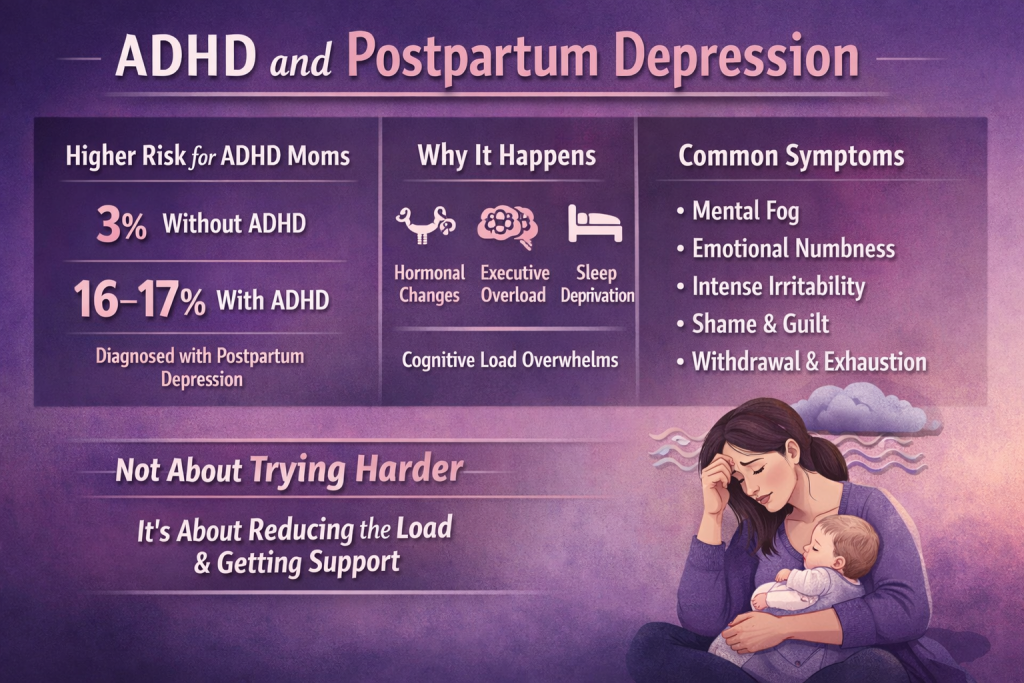
Large population studies show that:
-
About 3% of women without ADHD are diagnosed with postpartum depression
-
About 16–17% of women with ADHD are diagnosed with postpartum depression
Postpartum anxiety follows a similar pattern:
-
About 5% of women without ADHD
-
About 25% of women with ADHD
These differences remain even after researchers account for age, education, relationship status, socioeconomic factors, and prior mental health history.
ADHD itself functions as a clear risk factor during the postpartum period.
This increased risk is not because ADHD women care less, bond less, or try less.
It occurs because postpartum life places extreme demands on executive functioning at the exact moment hormonal support drops.
Why ADHD Significantly Increases Risk After Birth
ADHD affects attention regulation, task initiation, working memory, and emotional regulation.
The postpartum period demands:
-
Constant monitoring of cues and needs
-
Rapid task switching
-
Emotional regulation under stress
-
Functioning with severe sleep disruption
-
Continuous decision-making without recovery time
These demands are structurally harder for ADHD brains to meet without additional support.
This is not a motivation issue.
Trying harder does not resolve executive functioning overload.
Support and accommodation do.
ADHD Is a Neurodevelopmental Difference, Not a Personal Failure
ADHD is a neurodevelopmental difference involving dopamine regulation, executive functioning, and nervous system sensitivity.
After childbirth, estrogen levels drop rapidly.
Estrogen supports dopamine signaling, which is central to:
-
Attention
-
Task initiation
-
Emotional regulation
-
Cognitive flexibility
ADHD brains already rely on less stable dopamine signaling.
When estrogen drops, many ADHD women experience a sharp reduction in cognitive and emotional capacity.
At the same time, postpartum life introduces:
-
Severe sleep deprivation
-
Constant interruptions
-
Loss of routine and predictability
-
High emotional and sensory demand
This combination overwhelms executive functioning.
Postpartum depression often emerges not because of emotional weakness, but because the brain is operating under sustained load without adequate support.
For a broader overview of how ADHD interacts with pregnancy and early parenthood, see: ADHD and Pregnancy
What Postpartum Depression Often Looks Like in ADHD Women
In ADHD women, postpartum depression often looks different than expected.
Common experiences include:
-
Extreme difficulty thinking clearly or organizing thoughts
-
Worsening attention and memory problems
-
Emotional volatility or emotional flattening
-
Intense irritability or anger
-
Feeling incapable despite sustained effort
-
Increased shame and self-blame
-
Withdrawing from support because interaction feels cognitively effortful
These symptoms are frequently misattributed to:
-
Anxiety alone
-
Poor coping
-
“New mom stress”
-
Adjustment difficulties
When ADHD is not recognized, appropriate support is delayed.
This Is Not About Bonding, Gratitude, or Wanting Motherhood Enough
Many ADHD mothers describe:
-
Loving their baby but feeling emotionally numb
-
Wanting to function but being unable to initiate tasks
-
Feeling overwhelmed by decisions that seem simple to others
-
Feeling ashamed because effort does not translate into functioning
This is not a failure of attachment.
It happens because:
-
Executive functioning is overloaded
-
Emotional regulation systems are taxed
-
Cognitive recovery time disappears
In ADHD women, postpartum depression often presents as shutdown, paralysis, irritability, or mental fog, not just sadness.
Why Standard Postpartum Advice Often Fails ADHD Women
Much postpartum mental health advice assumes intact executive functioning.
Suggestions such as:
-
“Sleep when the baby sleeps”
-
“Lower your expectations”
-
“Practice self-care”
-
“Ask for help”
require planning, initiation, follow-through, and memory.
For ADHD women, the problem is not willingness.
It is executive functioning load.
Support must reduce cognitive burden, not add more tasks to manage.
This same systems mismatch often appears earlier in pregnancy and medical care.
Related reading: ADHD and Prenatal Care
What Actually Helps ADHD Women After Birth
Support that helps ADHD women during the postpartum period focuses on removing demands rather than increasing effort.
This often includes:
-
Proactive mental health monitoring during pregnancy and postpartum
-
Medication evaluation with clinicians familiar with ADHD and perinatal mental health
-
Explicit support plans rather than informal offers of help
-
Partners taking over cognitive labor, not just physical tasks
-
Reducing decision-making wherever possible
-
External structure that does not rely on memory or initiation
Medication decisions are individualized and should be discussed with knowledgeable providers.
More detail here: ADHD Medication During Pregnancy and Postpartum
Sleep disruption, feeding demands, and sensory load can further increase risk.
Related reading: ADHD and Breastfeeding

When to Seek Professional Support
If you experience:
-
Persistent low mood
-
Loss of functioning
-
Emotional numbness
-
Intrusive thoughts
-
Thoughts of harming yourself or your baby
This requires immediate professional support.
Postpartum depression is treatable.
ADHD does not disqualify you from recovery.
Medical Disclaimer
This content is for educational purposes only and is not a substitute for medical advice, diagnosis, or treatment. Postpartum depression and anxiety are medical conditions that require individualized care.
If you are pregnant, postpartum, or planning pregnancy, always consult a qualified healthcare provider before starting, stopping, or changing any medication or treatment. If you experience thoughts of harming yourself or your baby, seek immediate medical care or emergency support.
References
Baker, A. S., Wales, R., Noe, O., Gaccione, P., Freeman, M. P., & Cohen, L. S. (2022).The course of ADHD during pregnancy. Journal of Attention Disorders, 26(2), 143–148.
Andersson, A., Garcia-Argibay, M., Viktorin, A., Ghirardi, L., Butwicka, A., Skoglund, C., Madsen, K. B., D’Onofrio, B. M., Lichtenstein, P., Tuvblad, C., & Larsson, H. (2023). Depression and anxiety disorders during the postpartum period in women diagnosed with attention-deficit/hyperactivity disorder. Journal of Affective Disorders. https://doi.org/10.1016/S0165-0327(23)00085-X
Scoten, O., Tabi, K., Paquette, V., Carrion, P., Ryan, D., Radonjic, N. V., & Hippman, C. (2024).Attention-deficit/hyperactivity disorder in pregnancy and the postpartum period. American Journal of Obstetrics & Gynecology, 231(1), 18–28. https://doi.org/10.1016/j.ajog.2024.02.025





